Wegovy and Saxenda are GLP-1 medications that were initially developed to treat Type 2 Diabetes, which is a disease where the body struggles to manage sugar in the blood. Obviously, the GLP-1 medications are good at reducing sugar in the blood; however, they are also good at helping with weight loss. As a result, they are now approved for managing obesity without the presence of diabetes.
Of course, that led to many of my followers asking, ‘What happens when people who don’t have diabetes take Wegovy or Saxenda?’ Which is an excellent question.
Are individuals who use Wegovy at risk of having hypoglycemia or their blood sugar going too low? In case you have never hung out with someone who has diabetes this = no bueno! In the worst case scenario it could lead to death.
Let’s dive in.
Hypoglycemia – Signs and Symptoms
 Hypoglycemia is something we want to avoid. For your awareness, let me quickly review the signs and symptoms.
Hypoglycemia is something we want to avoid. For your awareness, let me quickly review the signs and symptoms.
If you have a glucometer at home (a machine that can measure the sugar in your blood), hypoglycemia is considered anything below 4.0mmol/L or 72mg/dL for my American friends. However, before you test and see those numbers, you are going to experience the symptoms first, which are:
- Shakiness, sweating, headache, hunger, fast heartbeat, anxiety, fatigue, difficulty concentrating, and dizziness.
If you have ever been ‘hangry,’ you have experienced mild forms of those symptoms. However, unless you are taking certain medications or have another medical condition, your body’s survival mechanisms will kick in and ensure the level of sugar in your blood does not go too low. You will just say mean and hurtful things to the people around you until you find some food.
So back to the question, can Wegovy, or Saxenda cause hypoglycemia?
The short answer is, No*.
There is an asterisk because there are exceptions. Plus, I enjoy cliffhangers, so hopefully, you are now hooked to keep reading and find out what those expectations are! #sorrynotsorry
Exceptions to the Rule: A Cliffhanger Journey
 In order to understand what the exceptions are, we need to briefly talk about how GLP-1 medications work. For a more in-depth review, check out this article.
In order to understand what the exceptions are, we need to briefly talk about how GLP-1 medications work. For a more in-depth review, check out this article.
GLP-1 medications mimic the GLP-1 hormone that is produced by our bodies. When you eat and that food hits your stomach GLP-1 gets released. GLP-1 manages blood sugars by increasing the level of insulin, increasing and/or preventing the breakdown of beta cells, slowing down gastric emptying, reducing sugar production by the liver, reducing appetite, and reducing insulin resistance.
So, let’s set the scene

You sit down to have a meal. Perhaps it is the meal you are eating right now over your lunch hour as you read my article. As you eat, GLP-1 gets released into the bloodstream.
First, it slows how quickly food moves from your stomach to your small intestine. This helps generate the signal, ‘the stomach is full. Stop eating.’
Simultaneously, GLP-1 heads to your pancreas and helps release insulin. Insulin is the main hormone that decreases the level of sugar in the blood. GLP-1 then sends out a signal to the liver to stop producing sugar, and instead start absorbing and storing the sugar that is entering the bloodstream from your meal. GLP-1 also chats with other cells in the body, such as your muscle cells and convinces them to become more sensitive to insulin so that sugar in the blood can be taken up easier – decreasing insulin resistance.
So the sugar in your blood is managed, you are no longer hangry and maybe even happy again. Then you go on with your day until you eat your next meal, and the process starts all over.
—
The beautiful part about the above processes, other than it all happens without you thinking, is that those mechanisms shut off when the sugar in your blood reaches a normal level, such as 2 hours post-meal. Therefore, whether it is the GLP-1 your body produces, or a GLP-1 medication, the level of sugar in your blood will never, in theory, go too low. That holds true for individuals that have and don’t have diabetes.
*Ok, what about the exceptions in taking a GLP-1 medication? 
These instances tend to be seen more in individuals with diabetes:
- Additional Anti-diabetes Medications
If an individual is on additional medications to manage their diabetes, in conjunction with a Wegovy or Saxneda, they are at an increased risk of experiencing hypoglycemia. The main offenders would be sulfonylureas (gliclazide, or glyburide), or insulin. These medications increase insulin levels, and they keep working even when blood sugar levels are in the normal range.
When a medication like Wegovy is added without proper medication adjustments, there is certainly a possibility of sugars going too low.
- Pseudohypoglycemia
This is an interesting phenomenon seen in people with diabetes.
If the level of sugar in your blood is consistently high, i.e. 15mmol/L or 270mg/dL and your blood sugar level is rapidly brought down towards the normal range 4-7mmol/L or 72-126mg/dL, you may experience symptoms of hypoglycemia.
However, when you test your blood sugar level, you find the level is above 4mmol/L or 72mg/dL. In this situation, the body is used to high levels of sugar, and when there is a sharp drop, it freaks out. There is too much change too quickly.
Like when I go away on a tropical vacation and come back to Canada in the middle of winter with -40 temperature, it takes at least two weeks to re-climatize, all while questioning why I live here.
- Idiopathic Hypoglycemia
This situation is rare, and I have seen it reported in individuals with and without diabetes.
Idiopathic means we don’t know what the cause is. In these cases, individuals are taking a GLP-1 medication and have no other factors present. Then the level of sugar in their blood may dip below the hypoglycemic level of 4.0mmol/L or 72mg/dL. While scary, it seems to be short-lived and not life-threatening as the body’s survival mechanisms kick in, and most will go eat when it happens.
From an anecdotal perspective with my patients, we may have found that it was linked to situations where the individual forgot to eat or went a significant amount of time without eating or was vomiting due to the side effects and being unable to eat. Either way, when we planned more structured and timed meals or snacks, the issue was resolved.
 If you don’t have diabetes, and even if you do but you are not on insulin or medications that release additional insulin, you don’t need to run out and buy a glucometer. You can if you want to, or it is recommended by your doctor.
If you don’t have diabetes, and even if you do but you are not on insulin or medications that release additional insulin, you don’t need to run out and buy a glucometer. You can if you want to, or it is recommended by your doctor.
However, if you focus on ensuring you are properly nourishing your body, all of the above can be easily mitigated! I hope it goes without saying but continue to follow up with your care providers as well.
For more information, check out these guidelines from Diabetes Canada on the management of hypoglycemia symptoms, and if needed, seek out immediate medical attention.
Anywho, to wrap things up, there are a few exceptions, even still, the GLP-1 medications are safe and effective!
—
Until next time my friends, always remember that small tweaks lead to massive peaks.
References:
Hypoglycemia low blood sugar in adults – https://guidelines.diabetes.ca/docs/patient-resources/hypoglycemia-low-blood-sugar-in-adults.pdf
Otherwise, always remember that small tweaks lead to massive peaks!
Until next time.
 Dr. Dan
Dr. Dan
Follow me on social media for regular updates – @TheOfficialDrDan
Subscribe to my newsletter for a heads-up on all new content.
Sharing is caring! Here’s the link for social, email, and even text – https://healthevolved.co/low-down-blood-sugar
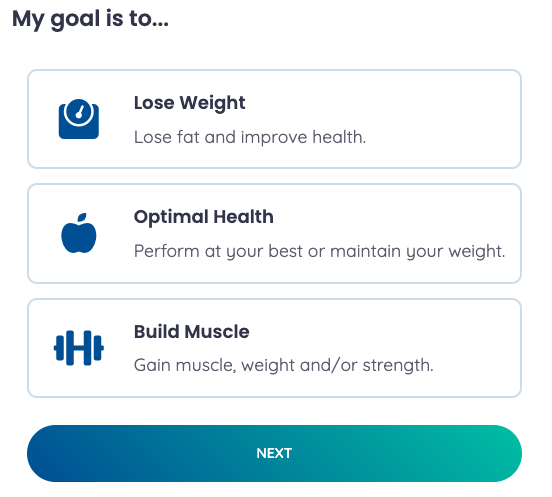
If you need some coaching support on your weight management journey, you can book a consultation with me to see if you’d be a good fit for our program.
Questions or comments? Please send them my way on our Contact Us page!



 Dr. Dan
Dr. Dan