When someone says they have diabetes, often they are referring to type 2 diabetes. Which is the most common form of diabetes. While all forms of diabetes are diseases that involve issues with managing sugar in the blood, there are some key differences between each of the types, how they develop, and how we treat them.
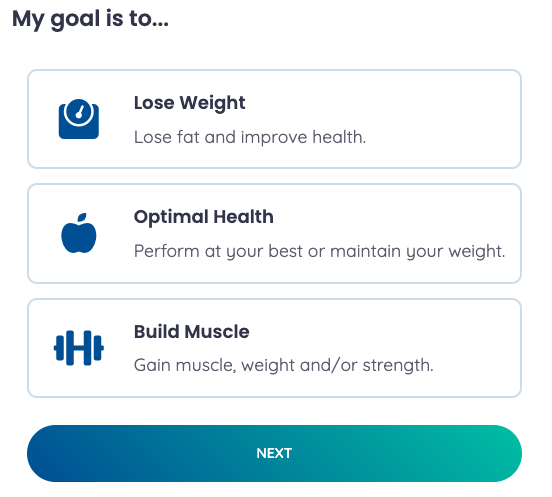
Fun fact – you may have only heard about diabetes types 1 and 2, but there are actually 7 other types of diabetes that an individual can develop.
The main organ involved in managing our blood sugars is the pancreas. The pancreas produces two hormones: insulin which brings the level of sugar in the blood down – after we have a meal, and glucagon, which brings the level of sugar in the blood up. Insulin is produced by special kinds of cells called beta cells.
The Immune System’s Role in Type 1 Diabetes: A Battle Against Beta Cells

Type 1 diabetes affects millions of people worldwide and, like almost every single disease on the planet, is due to a combination of genetic and environmental factors. The main driver of its development seems to be an individual’s own immune system waking up a little cranky one day and saying, ‘I don’t like the look of these beta cells. So I am going to get rid of them.’ Fortunately and unfortunately, the immune system is very good at wiping things out when it wants to. Obviously, this is great when we have an infection, but when it involves our own body, it tends to be ‘Bad News Bears.’
Eventually, these individuals have all of their beta cells wiped out, and they can no longer produce the necessary insulin to bring the sugar level in their blood down. They then become what we call insulin dependent. Which means they must inject insulin into their body multiple times per day. Individuals who have type 2 diabetes may also be on insulin; however, they are often on an array of other medications, such as Metformin, Jardiance, and Ozempic, that support blood sugar management as individuals that have type 2 diabetes tend to have residual beta cell function and can still produce their own insulin.
Balancing Risks and Benefits
Regardless, this begs the question as to why GLP-1 medications like Ozempic are not approved for the management of type 1 diabetes.
There are a couple of reasons for this.
- Part of the GLP-1 medication’s mechanism for reducing sugar in the blood is by supporting the pancreas to produce more insulin. If you have a pancreas that does not produce insulin, this mechanism probably won’t work very well.
- GLP-1 medications help to reduce blood sugars in other ways, too, such as reducing insulin resistance, decreasing sugar output from the liver, and reducing food intake, which should reduce carbohydrate intake.
- A study published in 2023 showed that when individuals with type 1 diabetes take a GLP-1 medication, there is ~0.7% reduction in A1C. Still a significant reduction but not quite as dramatic as what we see in people with type 2 diabetes – which can be upwards of a 2% decrease.
- Concerns with the development of hypoglycemia and/or diabetic ketoacidosis (DKA).
- If you have type 1 diabetes, you should, or at least I hope you have heard about DKA. If not, please review this article.
- DKA and hypoglycemia can be life-threatening conditions and are more often seen in people with type 1 diabetes. GLP-1 medications may contribute to the development of both.
 What we have is a situation where there is a potential for increased risk and maybe a marginal benefit. And the question clinicians like myself ask is, does the benefit outweigh the risk? When the GLP-1 medications first came to market, this was a tough call, and no clinicians really wanted to put their butts on the line.
What we have is a situation where there is a potential for increased risk and maybe a marginal benefit. And the question clinicians like myself ask is, does the benefit outweigh the risk? When the GLP-1 medications first came to market, this was a tough call, and no clinicians really wanted to put their butts on the line.
‘Today is the day I would like to be sued’, said no clinician ever.
Promising Evidence: Ozempic and GLP-1 Medications
However, further evidence has come out and can help to answer the question of whether we can use Ozempic and other GLP-1 medications in type 1 diabetes?!
The short answer is yes! While these drugs do not have the formal indication from the FDA or Health Canada, and I am not sure if they ever will, we now have some good data that shows GLP-1 medications are not only beneficial but are also safe in type 1 diabetes!

In terms of benefits, as I already mentioned, there were reductions in blood sugars, and some patients were also able to reduce their insulin doses. As well, some individuals reported weight loss and – depending on the review you look at, weight loss from baseline ranged from ~3.2-4.8kg (~7-10.5lbs).
Note: PLEASE, if you have type 1 diabetes, DO NOT come off your insulin. You need it to live. You might be able to reduce your doses with the addition of a GLP-1 medication, but you can never stop!
Safety Assurance: GLP-1 Medications
In terms of safety, there was no increased risk of hypoglycemia or DKA. Which is pretty darn cool but not necessarily unexpected. One thing to keep in mind is that the mechanisms by which GLP-1 meds reduce blood sugar actually shut off when blood sugar levels are in a normal range. Therefore, they will not continue to push sugar levels down inappropriately. Of course, close monitoring of blood sugar levels and adjustment of insulin dosages is very important!
 In summary, despite a rebellious immune system, GLP-1 medications seem to be not only effective but also safe to use in individuals with type 1 diabetes. For blood sugar management, it should be added to insulin therapy, and/or it can be used as an adjunct agent in supporting weight loss. With dietary and lifestyle changes, of course! So be sure to discuss this with your doctor, and if you are looking for a paper or two to share, check out the references below!
In summary, despite a rebellious immune system, GLP-1 medications seem to be not only effective but also safe to use in individuals with type 1 diabetes. For blood sugar management, it should be added to insulin therapy, and/or it can be used as an adjunct agent in supporting weight loss. With dietary and lifestyle changes, of course! So be sure to discuss this with your doctor, and if you are looking for a paper or two to share, check out the references below!
Until next time my friends, always remember that small tweaks lead to massive peaks!
 Dr. Dan
Dr. Dan
Follow me on social media for regular updates – @TheOfficialDrDan
Subscribe to my newsletter for a heads-up on all new content.
Sharing is caring! Here’s the link for social, email, and even text – https://healthevolved.co/type1-diabetes
If you need some coaching support on your weight management journey, you can book a consultation with me to see if you’d be a good fit for our program.
Questions or comments? Please send them my way on our Contact Us page!
References:
MDPI (February 6, 2023). A Review of the Effects of Glucagon-Like Peptide-1 Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors on Lean Body Mass in Humans. Retrieved from: https://www.mdpi.com/2673-396X/4/1/8
Centers for Disease Control and Prevention. (December 30, 2022). Diabetic Ketoacidosis. Retrieved from: https://www.cdc.gov/diabetes/basics/diabetic-ketoacidosis.html#print
Liu L, Shao Z, Xia Y, Qin J, Xiao Y, Zhou Z, Mei Z. Incretin-based therapies for patients with type 1 diabetes: a meta-analysis. Endocr Connect. 2019 Mar;8(3):277-288. doi: 10.1530/EC-18-0546.
Mohandas D, Calma J, Gao C, Basina M. Evaluating the Efficacy and Safety of Long-Acting GLP-1 Receptor Agonists in T1DM Patients. Endocrines. 2023; 4(1):93-101. https://doi.org/10.3390/endocrines4010008
Dejgaard TF, von Scholten BJ, Christiansen E, Kreiner FF, Bardtrum L, von Herrath M, Mathieu C, Madsbad S; ADJUNCT ONE and ADJUNCT TWO Investigators. Efficacy and safety of liraglutide in type 1 diabetes by baseline characteristics in the ADJUNCT ONE and ADJUNCT TWO randomized controlled trials. Diabetes Obes Metab. 2021 Dec;23(12):2752-2762. doi: 10.1111/dom.14532..
Guyton J, Jeon M, Brooks A. Glucagon-like peptide 1 receptor agonists in type 1 diabetes mellitus. Am J Health Syst Pharm. 2019 Oct 15;76(21):1739-1748. doi: 10.1093/ajhp/zxz179.


 Dr. Dan
Dr. Dan